
Invitation Only Scrubs to Business Program
Meet Our Official Sponsor

Empowering aspiring healthcare entrepreneurs with the tools, resources, and knowledge they need to start and grow their own businesses successfully. .
Launch Your Remote Care Management Venture
Transform your healthcare career with our innovative Scrubs to Business Program. Join a thriving community of healthcare professionals who have successfully launched care management businesses. Our program licenses cutting-edge software giving you access to an online training and business education portal, and personalized support to land contracts and own your own profitable Care Management Business.
Accepting New Applications
Have You Been Selected?
Have you wanted to start your own business?
Getting Started Is Simple:
Who We Work With:
Qualified LPN's RN's, NP's, and PA's
Business Oriented Healthcare Professionals
4-5 years' experience providing community-based patient care
Aspiring/Current Entrepreneurs who value qualities such as
integrity, compassion, innovation, and a commitment to improving healthcare outcomes
Multiple Payment Options Available:
Buy Now Pay Later Options with Klarna and Affirm
Pay in 3-4 interest free installments
Monthly Payment options for up
to 24 months.
What Our S2B Clients Are Saying
Why Choose ATD Healthcare Solutions?
Experienced Healthcare Executives:
Our team specializes in landing $500K to $2M care management contracts for RNs, PAs, NPs, and MDs.

Unique Business Model (Shared Success)
100% Retained Equity: Maintain full ownership of your business. Our success is a direct reflection of our clients' success. Our program is built around our ability to guide you into a business contract providing chronic care management services and remote patient monitoring services. This means that our profitability is directly tied to your ability to land and service contracts.
High Profitability and Scalability:
Achieve success and profitability with just one contract. Small contracts can generate $200k to $400k in revenue, while average private contracts range from $400k to $800k. Manage operations independently or scale with our support. Utilize our proprietary formulas and ROI analysis calculators for detailed cost and profit insights, ensuring maximum value delivery.
Comprehensive Support:
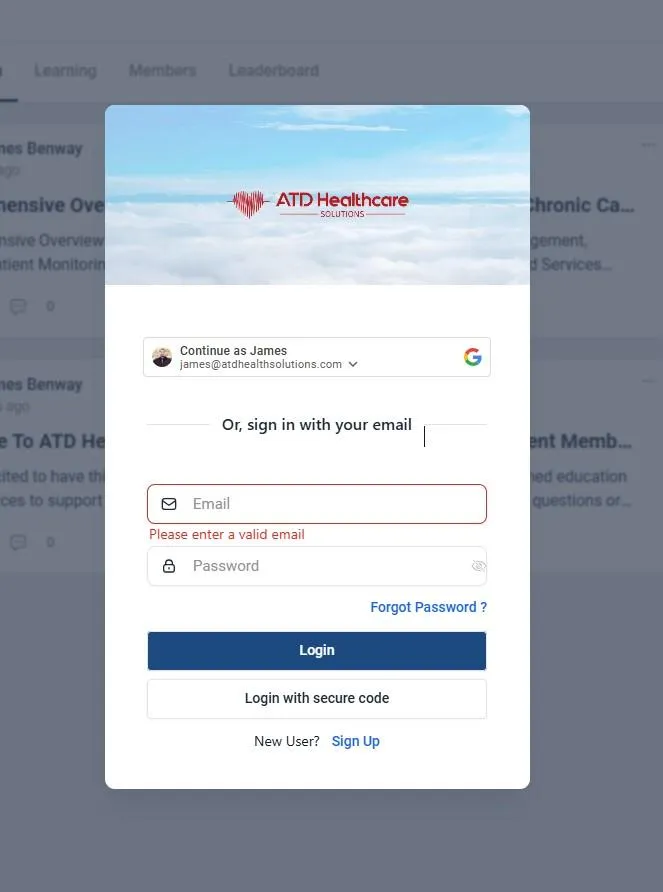
From helping you land new business to providing full membership access to our proprietary Scrubs to Business Proprietary training portal. You are able to have direct access to operational training, business startup guides, resources, and downloadable contract templates, we ensure you are provided comprehensive support. Additionally, as a care coordination SaaS licensor, we assist in closing and securing contracts, ensuring your growth at every step of your journey.

Done-for-You Solutions:
We provide customized presentation decks and business plan guidance tailored to each member, along with direct support in educating your potential provider clients and closing contracts.

How Does It Work
Our Program Is Simple, we have designed a straightforward 6-step process to ensure your you have all the tools you need to be successful. Our selective process allows us to ensure our subscribing members get the service and support they need to be well-prepared and a perfect fit for a long-term partnership with us.
Investment and Benefits
What Is My Investment
We are committed to your success, offering personalized 1-on-1 support from our team for 3 to 6 hours per month until you secure your first contract. Our goal is to establish a lasting partnership with you in Remote Care Management. By subscribing to our 1-year training program and becoming a Scrubs To Business Member, you invest in your career with comprehensive training and numerous benefits. This one-time payment of $1,997 covers the training program and reflects our commitment; if we do not help you secure a contract, we lose money, emphasizing our dedication to your success.
A wealth of knowledge and direct business development resources:
"Our proprietary business model, which you'll master through our training platform, combined with our extensive operational knowledge and training, forms the essential foundation for your success and profitability. Equipped with our tools and resources, you become the crucial piece needed to introduce effective care management to your local private practice community. Together, we enhance profitability and success. Your clinical expertise is invaluable, and we're here to empower you to leverage it and build a thriving business."
Exclusive Access and Personal Support:
Each subscribing member receives a unique reseller and user license, granting exclusive access to our proprietary Care Coordination/Management Software, essential for any successful Chronic Care Management Program. We provide personalized 1-on-1 support to assist you in securing contracts and thriving in your new career. Join us today and take the first step towards a successful future in chronic care management.
The 6 Steps To Success
#1 Apply to become a selected candidate
#2 If Selected Schedule Interview
#3 Purchase Launch Program One Time Subscription
#4 Custom Pitch Deck Creation + Implementation Meeting Scheduled Through Your Portal
#5 Full Access to A Dedicated Executive That Will Support You Towards Landing Your First Contract.
#6 Contract Landed and ATD Healthcare Solutions Software Licensing Partnership MSA Established.
Program Flyers and CMS/CCM Information Links
Online Membership Portal Access




Custom Designed Presentations and All in One Business Resources
Our program is designed to save you time providing you with resources that support your business startup.
Our industry proven pitch decks are designed and created to represent your business stuff
Have You Been Selected to Join Our Program?
Getting Started Is Simple:
Multiple Payment Options Available:
Buy Now Pay Later Options with Klarna and Affirm
Pay in 3-4 interest free installments
Monthly Payment options for up to 24 months
Frequently Asked Questions (FAQ's)
What are my potential annual earnings with a small contract?
Revenue Projections: Total patients: 300 (initial 150 + additional 150) Billed Codes: CPT 99490 + 99439(2).
Assumptions: Every patient will receive 60 minutes of care monthly, broken down as follows:20 minutes billed under CPT 99490. 40 minutes billed under two units of CPT 99439. This will require 1 additional staff member (LPN or RN).
Revenue Calculation:
Total Monthly Revenue: (CPT 99490) + (CPT 99439 first unit) + (CPT 99439 second unit) = $31,500
Annual Revenue: $31,500 * 12 = $378,000
Total Profit Estimated Calculation:
Monthly Profit: $17,166.67
Annual Profit: $206,000
What role do the physicians play in this?
General Supervision and Oversight: Physicians are responsible for the overall direction and control of the CCM program. They ensure that the clinical staff (CCM Company) adheres to the care plans and protocols established for each patient. Under "incident to" general supervision, the CCM Company can provide Clinical Staff services as long as they are under the physician's general oversight. This means the physician must be available to provide assistance and direction but does not need to be physically present during the provision of services.
How are patients enrolled into the program?
Physicians or supervised clinical staff (CCM Company) must obtain and document the patient's consent to participate in the CCM program. This consent can be verbal or written and must be recorded in the EHR.
Does the patient have to pay for anything out of pocket regarding co-insurance?
Patients with medicare and a secondary as well as medicare advantage are typically covered 100%. For Patients with Medicare only and no secondary insurance might be responsible for a co-insurance payment, which typically is 20% of the CCM service cost after the annual Part B deductible is met. Average co-pay is estimated around $15 to $25 per patient.
Do I need a business plan?
Yes, having a business plan is always beneficial as It outlines your business goals, strategies, market analysis, financial projections, and operational plans. This can help to secure financing, attract partners, and guide the growth of your CCM business. Part of our program is helping you do develop and finalize your personal business plan when it becomes necessary.
If I decide to hire an additional Care Manager (RN, LPN) how much profit would I make?
Hiring additional nurses allows you to handle more patients and thus increase profits. Each additional nurse can manage approximately 120 to 150 patients, generating an estimated 40k to 60K in profit per year.
Are there payment plans available to get started?
Yes, our mission is to break down the barriers that are preventing healthcare professionals like you from beginning their journey into their own business. We partner with Karna and Afterpay which offers you the ability to pay in 3-4 interest free installments or financing up to 36 months.
What is my total investment?
Our program is designed with a singular focus: we succeed when you succeed. We only charge a onetime end user licensing fee of $1,997 to participate in our Scrubs to Business Program. This allows full access to our software for you to use under your brand. We understand that our success is tied to your ability to land your first contract. This drives us to provide you with exceptional support. With our competitive advantage and top-notch sales support, we aim to help you secure your first contract. Allowing us to contract together servicing your clients successfully while building a long-term prosperous partnership. Other small costs that you may have to cover are little things like entity registration, insurance, email, home office equipment (if needed). Our portal has affordable resources simplifying your start up business process.
Will I need a website?
A professional website is not needed but can always add value. We can build a simple website for you if you feel that it's something you will need; However, we substitute that with a live digital presentation deck that is visible online to all of your potential practice/providers.
How long is the training and how long will it take for me to feel comfortable contacting practices/providers?
The great thing about our program is we go at your pace; however typically, the initial training course can be completed in 1-2 weeks. This includes learning the software, understanding CMS guidelines, and developing sales strategies. Registering your business and ensuring you are properly set up can take 3 to 6 weeks.
Operational Timeline: From the start of training to contacting physicians and onboarding patients, it can take an estimated 1 to 3+ months to land a contract if you have great connections or 3-6+ months without connections. Once a contract is signed you typically start on the 1st or the 15th on any given month which is about 1 to 2 weeks after contract signing which is (recommended); however, you can start any time after your contract is signed.
What is Chronic Care Management (CCM)
Chronic Care Management (CCM) refers to the coordinated care provided to patients with multiple chronic conditions that are expected to last at least 12 months or until the patient's death. This care aims to manage and improve health outcomes, decrease hospitalizations, and enhance the overall quality of life for patients.
Key Aspects of Chronic Care Management:
Patient Eligibility: Patients with two or more chronic conditions expected to last at least 12 months or until death. Conditions that place the patient at significant risk of death, acute exacerbation, or functional decline.
Service Providers: Physicians and certain non-physician practitioners (e.g., Nurse Practitioners, Physician Assistants). Rural Health Clinics (RHCs) and Federally Qualified Health Centers (FQHCs). Hospitals, including Critical Access Hospitals.
Care Coordination Activities: Developing a comprehensive care plan. Managing care transitions and coordination among providers. Providing access to care outside of regular office visits. Continuous monitoring and communication with patients. Use of Electronic Health Records (EHRs) for tracking patient data.
Benefits of CCM: Improved patient engagement and education about their conditions. Better management of chronic diseases and health outcomes. Increased patient satisfaction and compliance. Reduced hospitalizations and emergency department visits. Additional revenue streams for healthcare practices through billing for CCM services.
Operational Workflow: Identify and enroll eligible patients with the provider's approval. Develop and implement a care plan. Conduct regular follow-ups and updates to the care plan. Provide continuous support and monitoring through clinical staff or CCM companies. Document and report compliance and billing information.
Billing and Reimbursement: CCM services can be billed monthly for non-face-to-face care coordination. Different billing codes apply based on the complexity and time spent on care management (e.g., CPT codes 99490, 99439, 99487). By implementing CCM programs, healthcare providers can enhance patient care, reduce healthcare costs, and create sustainable practice revenue through effective chronic disease management.
What is BHI?
In Behavioral Health Integration (BHI), a care manager plays a crucial role in coordinating and managing a patient's overall care. Here are the key responsibilities and activities performed by a care manager:
Assessment and Planning: Conduct comprehensive assessments of patients' behavioral and physical health needs. Develop individualized care plans that address both mental health and physical health conditions.
Care Coordination: Facilitate communication and collaboration among primary care providers, behavioral health specialists, and other healthcare professionals. Ensure that all members of the healthcare team are informed about the patient's treatment plan and progress.
Patient Support and Education: Provide education and resources to patients and their families about managing their conditions. Offer support and counseling to help patients adhere to their care plans and make necessary lifestyle changes.
Monitoring and Follow-Up: Regularly monitor patients' progress and response to treatment through follow-up appointments and check-ins. Adjust care plans as needed based on patients' changing health status and feedback.
Crisis Intervention: Respond to urgent behavioral health needs and coordinate appropriate interventions. Assist patients in accessing emergency services if necessary.
Documentation and Reporting: Maintain accurate and up-to-date patient records, including assessments, care plans, progress notes, and communication logs. Report on patient outcomes and care effectiveness to the healthcare team and relevant stakeholders.
Advocacy and Resource Coordination: Advocate for patients' needs within the healthcare system and community. Connect patients with additional resources and services, such as social services, support groups, and financial assistance programs. The care manager ensures that patients receive comprehensive, coordinated care that addresses both their physical and mental health needs, leading to better health outcomes and improved quality of life.
How does CCM improve patient outcomes?
CCM improves patient outcomes by providing structured, continuous care that addresses all aspects of a patient's health. This includes regular monitoring, personalized care plans, and enhanced communication between patients and healthcare providers. These efforts lead to better management of chronic conditions, reduced hospitalizations, and fewer emergency visits.
What are the financial benefits for providers who contract with me to manage their CCM?
Providers benefit financially from implementing CCM through increased revenue from billing for CCM services using specific CPT codes. Additionally, improved patient outcomes and satisfaction can lead to higher patient retention and attract new patients, further enhancing the practice's revenue. We teach you what the profit margins are and how to set competitive pricing to ensure long term sustainability for both you as a CCM company and the Provider as your client.
Reimbursement for CCM services through specific billing codes (e.g., CPT codes 99490, 99439, 99487).: Profit ranges from $50,000k to $90,000K per year per 150 patients depending on whether they are an NP, PA, MD, DO. Average Profit per small private practice with only 300 patients enrolled is around 140,000+ per year
Increased practice revenue from improved patient retention and new patient attraction.
Potential for additional payment for managing high-risk, high-needs patients.
What evidence supports the effectiveness of CCM?
Studies and data from the Centers for Medicare & Medicaid Services (CMS) show that CCM services reduce hospitalizations by nearly 5% and emergency department visits by 2.3%. Providers also report improved patient satisfaction, adherence to recommended therapies, and enhanced clinician efficiency.
How does the care manager facilitate communication among the healthcare team?
The care manager facilitates communication by Coordinating between primary care providers, specialists, and other healthcare professionals. Ensuring all team members have access to the patient’s care plan and updates. Scheduling regular team meetings and using EHR systems to share information. Acting as the main point of contact for patients and providers.
How does CCM support the overall growth and sustainability of a healthcare practice?
CCM supports growth and sustainability by enhancing patient outcomes and satisfaction, leading to better patient retention. It also provides an additional revenue streams through CCM billing and Improving practice efficiency and clinician satisfaction as well as Strengthening the practice’s reputation for providing comprehensive, high-quality care.
What types of chronic conditions qualify for CCM?
Qualifying conditions include, but are not limited to, diabetes, hypertension, heart disease, asthma, arthritis, chronic obstructive pulmonary disease (COPD), and mental health disorders.
What are the billing codes used for CCM services, and average reimbursement to providers used for CCM services, and how are they applied?
Common Billing codes for CCM services include:
CPT 99490: For non-complex CCM, which involves at least 20 minutes of clinical staff time per month. The national average reimbursement is approximately $64.51.
CPT 99439: For additional 20-minute increments of non-complex CCM. The national average reimbursement is approximately $47.35.
CPT 99487: For complex CCM, requiring at least 60 minutes of clinical staff time per month. The national average reimbursement is approximately $133.76.
CPT 99489: For each additional 30 minutes of complex CCM. The national average reimbursement is approximately $70.60. These codes are applied based on the time spent and the complexity of the care provided.
The Practices that I have relationships with manage their own CCM program can I still bring them value? Why would they stop managing it themselves and choose to contract with me?
Yes, you can bring value to practices that manage their own Chronic Care Management (CCM) programs. Here are several reasons why they might consider contracting with you instead:
1. Expertise and Efficiency: We specializes in landing high-earning care management contracts as well as our offering of extensive support services. This includes providing efficient care coordination software, which streamlines operations and enhances care quality. By partnering with ATD, you can leverage our software, education and training portal and care management expertise to ensure your company is seen as an expert in the CCM space which allows you to improve their program efficiency and patient outcomes.
2. Comprehensive Care Coordination Software: Your Care Coordination Software offers features that more than likely surpasses the existing tools of the practices. These include:
-Automated Documentation: Simplifies the creation and maintenance of patient records and billing reports allowing for simplicity and compliance. Most practices that are running internally are struggling with compliance or are non-compliant.
-Patient Interaction Tracking: Enhances the ability to monitor and manage patient interactions effectively.
-HIPAA-Compliant Security: Ensures that patient data is protected according to the highest standards.
3. Reduced Operational Burden and Scalability: Managing a CCM program in-house can be resource-intensive. By outsourcing to a specialized company, practices can reduce their operational burden. This allows them to focus more on direct patient care rather than administrative tasks. Most private practices are only enrolling and managing around 100 patients for every 1,000 patients which would bring them in $7000 to $9000 in profit per month (this is not accounting for operational training costs and turnover costs which is high for private practices). A Contracted CCM company due to their software and operational processes are able to manage 2 to 4 times ($8,000 to $16,000) that amount leading to more profitability and increased operational efficiency and patient outcomes while also allowing for more of their patient population to be able to participate in a program that they should have access to.
4. Financial Benefits: Outsourcing can lead to significant cost savings. You company offers competitive pricing which can be more cost-effective compared to managing a full-scale CCM program internally. Additionally, practices can benefit from improved billing and claims management, ensuring they capture all possible revenue.
5. Enhanced Patient Care: By partnering with a CCM company, practices can ensure that their patients receive continuous and comprehensive care management. This includes structured recording of patient health information, and comprehensive care plans that support disease control and health management goals.
6. Regulatory Compliance: Staying compliant with CMS guidelines and other regulatory requirements is critical. Your program and software partnership with ATD gives the provider a peace of mind that all of their CCM services adhere to current regulations, which can mitigate the risk of non-compliance penalties for practices.
7. Support and Training: You are able to offer support and training to ensure that all provided care management staff are well-equipped to use the care coordination software and manage the CCM program effectively. This includes regular updates and training sessions to keep your staff informed about the latest best practices and regulatory changes.
Summary: By contracting with you, practices can enhance their CCM programs through improved efficiency, reduced operational costs, enhanced patient care, and robust regulatory compliance. Your expertise and comprehensive service offerings make it an attractive option for practices looking to optimize their care management efforts.
How does ATD Healthcare Solutions make a profit?
Our profitability is directly tied to your success and ability to land and manage a contract. Through our program you are licensed software that allows you to service your customers and drive increased efficiency, compliance, and data recording for optimizing care management outcomes. This is a per user cost that will be paid to us on a monthly basis. Once the provider pays you then you are paying ATD for each user on the platform. Allowing you to drive an estimated 80% to 90% profitability margin for your first 150 patients.
Who bills for these services if I am contracted with a provider/practice?
The billing and reimbursement processes are typically handled as follows:
Clinical Staff Involvement: The clinical staff under the general supervision of the healthcare provider (Your Company) delivers the CCM services. This involves care coordination, patient monitoring, and other relevant activities.
Software Integration: All patient interactions, care plans, and documentation are recorded using your Care Coordination Software, which ensures that the documentation meets CMS requirements.
Billing Submission and Claims Preparation: Your Software helps with the preparation of billing claims by ensuring that all services provided are accurately documented and coded. At the end of every month your software creates a simple billing summary report that allows the providers billing team to comfortably and compliantly bill for each rendered service.
Submission to Payers: The healthcare providers billing team submits these claims to the relevant payers, such as Medicare, Medicaid, or private insurers.
Reimbursement Process: The healthcare provider directly receives the reimbursement from the payers. This includes payments for CCM services provided under the CMS guidelines and any other covered services.
Revenue Sharing and/or Cost-Sharing Arrangement: There is a predetermined cost-sharing arrangement between the healthcare provider and the contracted CCM company (i.e., Your Care Management Company). This arrangement specifies the pre-determined portion of the reimbursement that is allocated to you for the services provided.
Invoice and Payment: You invoice the healthcare provider for services rendered as per the terms outlined in your contract with the practice (Master Services Agreement (MSA)).
Summary of Responsibilities of the Healthcare Provider: Provides general supervision of clinical staff (your company) included but not limited to approval and revision of all care plans and Submits claims to payers. Receives reimbursements directly from payers. Pays your company for their share of the revenue based on the cost-sharing agreement.
Your Contract responsibility: utilizes end user care coordination software and provides clinical staff support. Assists with billing documentation and claims preparation via generated billing summary reports. Invoices the healthcare provider for their portion of the reimbursement.
This structured approach ensures that all billing is handled efficiently, and reimbursements are appropriately shared, allowing both the healthcare provider and your company to benefit from the partnership.

Follow Us
Follow Us
Care Coordination Software Licensing, value added consulting, online portal including training modules, resources, and support for starting and managing chronic care management programs and businesses. Access to our educational portal includes, custom developed presentation decks, CCM, PCM, RTM, RPM, and BHI business educational content and tutorials, Industry standard resources, contracting education. Additionally, our membership offers complimentary expert consulting services, including sales and contracting closing support streamlining our clients into business. Giving you the unique opportunity of a partnership/contract with us to support the success of your business with our care coordination software licensing platform and online business development membership.
Services
More
© Copyright 2025. ATD Healthcare Solutions. All rights reserved.
